| Posted: Jun 24, 2014 |
Carbon nanoparticle assisted photothermal delivery using laser light
|
|
(Nanowerk News) UT Arlington physics researchers may have developed a way to use laser technology to deliver drug and gene therapy at the cellular level without damaging surrounding tissue. The method eventually could help patients suffering from genetic conditions, cancers and neurological diseases.
|
|
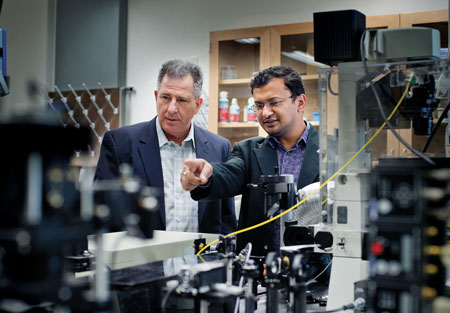
In a study published recently by the journal Nature Scientific Reports ("Crystalline magnetic carbon nanoparticle assisted photothermal delivery into cells using CW near-infrared laser beam"), the team paired crystalline magnetic carbon nanoparticles and continuous wave near-infrared laser beams for in what is called photothermal delivery. Authors of the new paper are Ali Koymen, a professor of physics; Samarendra Mohanty, an assistant professor of physics; and Ling Gu, a researcher in Mohanty’s lab.
|
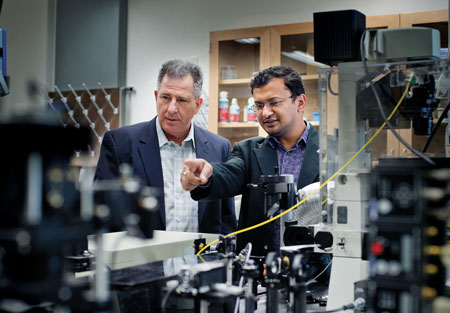 |
| Physics Professor Ali Koymen, left, and Samarendra Mohanty, an assistant professor of physics, discuss their research.
|
|
The new discovery grew out of previous study where Koymen and Mohanty used a 50 to 100 milliwatt laser and the same carbon nanoparticle, which absorbs the beam, to heat up and destroy cancer cells in the lab. The team used the new photothermal delivery method in lab experiments to introduce impermeable dyes and small DNA molecules into human prostate cancer and fibroblast sarcoma cells.
|
|
“In this work, Dr. Mohanty used a lower power, 20 to 30 milliwatt, continuous wave near-infrared laser and the nanoparticle to permeate the cell membrane without killing the cells. This method stretches the desired cell membrane to allow for delivery and has the added bonus of creating a fluid flow that speeds the movement of what is being delivered,” said Koymen, whose lab created the study’s crystalline magnetic carbon nanoparticle using an electric plasma discharge inside a toulene solution.
|
|
Introducing foreign DNA or other small molecules directly into cells is essential for some of the most advanced methods being developed in gene therapy, vaccinations, cancer imaging and other medical treatments. Currently, the predominant practice is using viruses for delivery to cells. Unfortunately, the scope of what can be delivered with viruses is severely limited and virus interaction can lead to inflammatory responses and other complications.
|
|
Scientists looking to create a path into the cell without employing a virus also have experimented with using UV-visible light laser beams alone. But that method damages surrounding cells and has a relatively shallow level of effectiveness.
|
|
A significant advantage of the new method is that the near-infrared light absorption of the nanoparticle can be used to selectively amplify interaction of low power laser with targeted tissue and “laser induced-damage to non-targeted cells along the irradiation path can be avoided,” the report says. The magnetic properties of the nanoparticles also mean they can be localized with an external magnetic field; therefore a smaller concentration can be used effectively.
|
|
|
|
“Research universities like UT Arlington encourage faculty and students to follow each new discovery with even deeper questions,” said Pamela Jansma, dean of the UT Arlington College of Science. “With their latest publication, Drs. Koymen, Mohanty and Gu have taken their collaboration to a new level as they keep building toward valuable implications for human health and disease treatment.”
|
|
Carbon nanoparticles produced for the cancer study varied from five to 20 nanometers wide. A human hair is about 100,000 nanometers wide. The magnetic carbon nanoparticles also are fluorescent. So, they can be used to enhance contrast of optical imaging of tumors along with that of MRI.
|