| May 16, 2012 |
Detecting tumour cells individually
|
|
(Nanowerk News) Sometimes, a tumour only develops very slowly. It begins with a few cells that mutate. Then these cells mutate. And mutate again. The mutants are more successful than their predecessors, outcompeting them as they multiply. Consequently, new variants of cells keep emerging, each fitter than their predecessors: the tumour goes through an evolution that gives rise to a genetically heterogeneous cancer.
|
|
This makes it difficult to treat a tumour with medication as there might be cells that do not respond to the drug used. Researchers from ETH Zurich and the Swiss Institute of Bioinformatics thus teamed up with colleagues from the University of Zurich to develop a new method for determining the genetic variants of tumour cells reliably. Using this method, the researchers are able to detect mutations that only appear in one in every 10,000 cells.
|
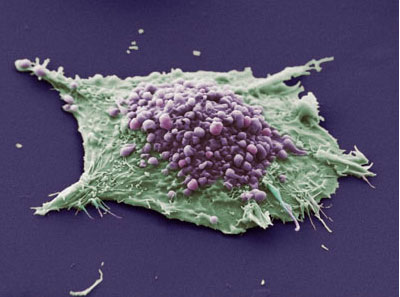 |
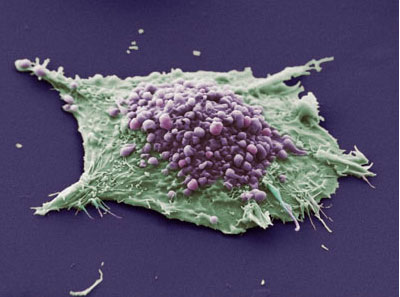
| A tumour consists of more different genetic variants of cancer cells (in the picture, a lung-cancer cell) than originally believed. (Photo: Wellcome Images / Flickr)
|
|
Test on renal cancer tissue successful
|
|
"This method will be important for use in clinics, for instance, when therapy-resistant cell types need to be detected to adapt the treatment accordingly," says lead author Moritz Gerstung from ETH Zurich's Department of Biosystems Science and Engineering. The study has just been published in Nature Communications ("Reliable detection of subclonal single-nucleotide variants in tumour cell populations").
|
|
The new approach also enables to measure the frequency of certain variants within the tumour-cell population, which sheds light on how tumours grow and how quickly they change genetically inside the patient.
|
|
In a comparison of two particular regions of two genes from healthy renal cells and renal cancer cells, the researchers found twenty-four gene variants. Some variants were only present in two in every 10,000 cells examined; others, however, in over a third.
|
|
Statistics compensate for read errors
|
|
For their method, the researchers genetically analyzed countless tumour cells from renal cancer tissue using a modern sequencing technique called "deep sequencing". As a result, millions of DNA fragments from single genes were sequenced simultaneously. These DNA fragments are isolated from the entire population of tumour cells and shed light on the genetic composition of the tumour. These genes were sequenced over 100,000 times, which corresponds to equally as many individually sequenced cells.
|
|
In reading the genetic code, however, errors can occur. So as not to mistake these errors for actual mutations, the researchers sequenced healthy tissue in parallel to be able to determine the error rate at any point on the DNA. In order to distinguish actual mutations from sequencing errors at a particular point, they developed a special statistical algorithm. "This was a critical step for us as even the tiniest of inaccuracies can cause a large number of errors because the algorithm analyses several million DNA fragments," says Dr. Gerstung.
|
|
Personalised cancer medicine the aim
|
|
The researchers began by testing their new method on control samples with a known cell composition to make sure that it worked and did not display any false forecasts. Then they analysed four tumour samples and found numerous mutations or subtypes cells. "Their existence supports the theory that tumours change constantly in accordance with a Darwinian evolutionary process," says Dr. Gerstung.
|
|
The new method helps personalise cancer therapy further. In future, tumours may not be treated as a unit. If one knows which cell types a tumour contains, the therapy can be adapted individually to a specific combination of drugs. When and whether the method will be used routinely in clinics remains to be seen. Further research is required to determine how tumour cell populations respond to different treatments. "However, the method is already at a stage where it can be also used for other cancer types," says the ETH-Zurich researcher.
|