| Nov 22, 2012 |
Biomedical engineering: technology that drives medical advances
|
|
(Nanowerk News) Systems to improve patient rehabilitation, methods that help detect diseases, and smart biomaterials for optimising treatments—scientific advances in the field of biomedical engineering are unstoppable. A number of leading UPC teams are carrying out research aimed at harnessing technology to improve people’s health.
|
|
Parkinson’s disease is the second most common neurodegenerative disease after Alzheimer’s. Optimising treatment and rehabilitation of the people it affects and improving their quality of life is the goal of Joan Cabestany and Andreu Català, researchers at the Technical Research Centre for Dependency Care and Autonomous Living (CETpD) of the Universitat Politècnica de Catalunya · BarcelonaTech (UPC).
|
|
The two engineers are heading up a European project known as REMPARK (Personal Health Device for the Remote and Autonomous Management of Parkinson’s Disease), which has a budget of €4.73 million. The objective is to develop a pioneering wearable monitoring system that can be used to identify and quantify, in real time and with high reliability, the motor status of Parkinson’s patients during their everyday lives. The system will act automatically—though always under medical supervision—in response to the situations that are most incapacitating for patients, intervening in the least invasive and most effective way possible. Other participants in this ambitious project coordinated by the UPC include the Teknon Medical Centre, Telefónica R&D, the European Parkinson’s Disease Association, and a number of research centres and companies based in Germany, Portugal, Italy, Israel, Ireland, Sweden and Belgium.
|
|
The system being developed consists of two elements: a bracelet equipped with a sensor for measuring tremor in patients and a smart device the size of a mobile phone, which is worn at the waist on a belt made of biocompatible material. The device is equipped with a set of sensors and has the capacity to process and wirelessly transmit all the information collected and processed.
|
|
When a gait-freezing episode occurs, the REMPARK system will act to synchronise the patient’s movements. This will be achieved by means of auditory, visual or haptic (touch-related) cueing devices, a pump for regulated subcutaneous drug delivery, and a functional electrical stimulation (FES) system. “The device will make it possible to quantify the effects of a drug in a particular patient and adjust the dose accordingly,” says Joan Cabestany, stressing that REMPARK is “a personalised system that adapts to each person’s needs.”
|
|
For the first time in Europe, REMPARK will be tested on a hundred patients in their homes. “We want to use the technology to give Parkinson’s patients back their confidence, which is gradually eroded by the disease,” says Andreu Català. The project “will reduce the number of hospitalisations and improve patient treatment and rehabilitation,” adds the researcher, who works at the Vilanova i la Geltrú Campus.
|
|
Stress-free cells
|
|
The REMPARK project is set to run until 2015, but others are yielding results that are about to hit the market. This was clear at the BIO International Convention, the world's largest biotechnology exhibition, which was held in Boston (Massachusetts, United States) last June.
|
|
The UPC presented a number of patents at the event, including an automatic method for introducing substances such as drugs and DNA into cells (transfection). The method, known as in vitro electroporation, is more efficient and economical than existing approaches.
|
|
The technique, which is applied manually, is commonly used in gene therapy, cell-based therapies, and tumour treatment by electrochemotherapy. Cells are detached from the bottom of the plates where they are grown and put into suspension, i.e. into a mixture. They are then placed in a special cuvette with aluminium electrodes on its sides. The cuvette is loaded into a device (an electroporator) that creates a high-intensity electric field across the cells, causing the pores in the cell membrane to open. Substances can then be introduced through these pores.
|
|
The new system simplifies and automates this process. A microelectrode assembly is introduced directly into the culture plate and placed at a distance of 10 ìm (10 millionths of a metre) from the cells. A 20 V electric field is then applied (in the conventional process a 500 V field is used). The lower voltage reduces the cost of the devices used to carry out these biotechnological processes and subjects the cells to less stress. The low cost of the microelectrodes also makes it possible to produce single-use electroporators. This patent was developed by researcher Ramon Bragós and doctoral student Tomàs Garcia, who are attached to the Biomedical Engineering Research Centre (CREB), in collaboration with a team at the University of Barcelona (UB).
|
|
The UPC is also contributing to major advances in the development of medical devices and diagnostic imaging. The UPC’s Institute of Industrial and Control Engineering (IOC) and the Pulmonology Research Group of Bellvitge Hospital’s Institute for Biomedical Research have developed a virtual bronchoscopy system that improves the diagnosis of lung cancer. The technology provides doctors with information that enables them to decide with more confidence whether an actual bronchoscopy is necessary or not. This helps minimise risk and discomfort for patients.
|
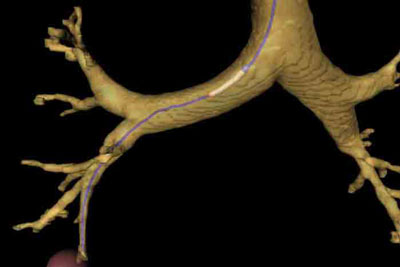 |
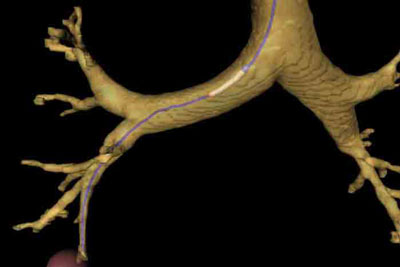
| Virtual bronchoscopy image, created using a system developed by the IOC that enables doctors to navigate virtually through a patient’s airways and diagnose lung cancer.
|
|
The system is based on images provided by a virtual bronchoscopy using 2D computed tomography images. The novel feature of the system is that it takes into account the geometry and kinematic constraints of the bronchoscope.
|
|
The device is designed so that a pulmonologist can virtually navigate through a patient's airways and simulate the movements that will later be executed when a flexible bronchoscope is used to perform the examination. It is a useful tool that facilitates “very realistic planning of the most feasible path from the trachea to peripheral pulmonary lesions,” says Jan Rosell, the researcher who carried out the project together with Paolo Cabras and Alexander Pérez, who also work with the IOC. “Doctors can also use the device to determine whether the end of the bronchoscope will reach a lesion, or, if not, how close it can be manoeuvred and what technique will need to be used to obtain a biopsy sample,” Rosell adds.
|
|
In addition to pursuing advances in diagnostic imaging, molecular biology and telemedicine, UPC researchers are also doing innovative work in another area of interest: metabolomics, the scientific study of chemical processes involving metabolites. It is in this field that another CREB team has patented an innovative software tool. The advanced program, based on a new algorithm, helps medical professionals make more accurate, automated predictions in disease diagnosis and drug screening.
|
|
Developed by Àlex Perera and Francesc Fernández in collaboration with researchers with the University of Barcelona’s Department of Nutrition and Food Science, the tool improves detection of biomarkers, the biological markers used to detect diseases.
|
|
Another advantage of the software is that it reduces prediction error in metabolomic analysis and testing (used to examine the small organic molecules in biological systems). Metabolomic analyses are based on biological samples of urine or blood, nuclear magnetic resonance (NMR) techniques, and mass spectrometry (LC/MS). Making predictions in this area is complex because it requires analysis of extensive data obtained from individual samples, but it is of vital importance in evaluating the effectiveness of new drugs, for example.
|
|
New test for tuberculosis
|
|
Tuberculosis is one of the diseases that accounts for the most morbidity and mortality worldwide. Despite this, there are still a lot of unanswered questions about the disease and many scientific challenges remain to be tackled. Daniel López Codina and Clara Prats of the UPC’s Discrete Modelling and Simulation of Biological Systems group have carried out research in this field in collaboration with a team at the Experimental Tuberculosis Unit of the Germans Trias i Pujol Health Sciences Research Institute Foundation.
|
|
The two teams have patented a new method that offers a fast, easy and reliable way to determine the virulence (ability to produce disease) of Koch's bacillus. The technique allows specialists to make more accurate diagnoses.
|
|
López Codina’s team observed the tuberculosis bacillus (Mycobacterium tuberculosis) in an in vitro culture and looked at the way it grows by forming clumps. Given the difficulty of applying conventional microbiological methods with this type of culture, the researchers used an alternative approach: microscopy and analysis with image processing techniques. “This is the first time we’ve been able to use a culture to observe two different strains of the bacterial parasite and the existence of a correlation between the characteristic clumping pattern and the virulence of the disease,” said the researcher.
|
|
The results have created a new business opportunity for companies involved in biomedical imaging and diagnostic testing.
|
|
Projects like these highlight the huge potential of engineering and medicine to continue delivering solutions that improve people's quality of life.
|