| Nov 09, 2015 |
Flipping the switch to better see cancer cells at depths
|
|
(Nanowerk News) Using a high-tech imaging method, a team of biomedical engineers at the School of Engineering & Applied Science at Washington University in St. Louis was able to see early-developing cancer cells deeper in tissue than ever before with the help of a novel protein from a bacterium.
|
|
Lihong Wang, PhD, the Gene K. Beare Distinguished Professor of Biomedical Engineering at the School of Engineering; Junjie Yao, PhD, a postdoctoral researcher in Wang's lab, and a team of engineers found that by genetically modifying glioblastoma cancer cells to express BphP1 protein, derived from the rhodopsuedomonas palustris bacterium, they could clearly see tens to hundreds of live cancer cells as deep as 1 centimeter in tissue using photoacoustic tomography.
|
|
The work, published Nov. 9 in advanced online publication of Nature Methods ("Multi-scale photoacoustic tomography using reversibly switchable bacterial phytochrome as a near-infrared photochromic probe"), is the first to combine deep-penetration, high-resolution photoacoustic tomography with a reversibly switchable, non-fluorescent bacterial phytochrome.
|
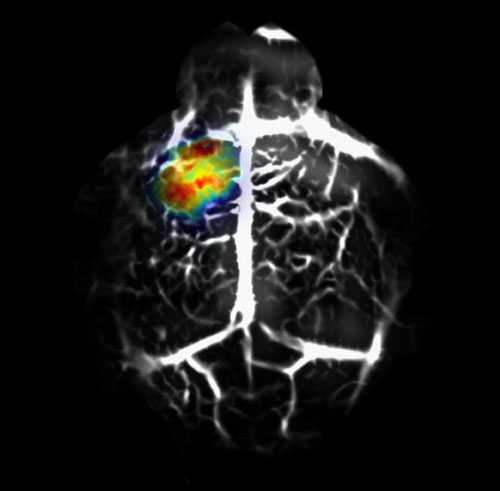 |
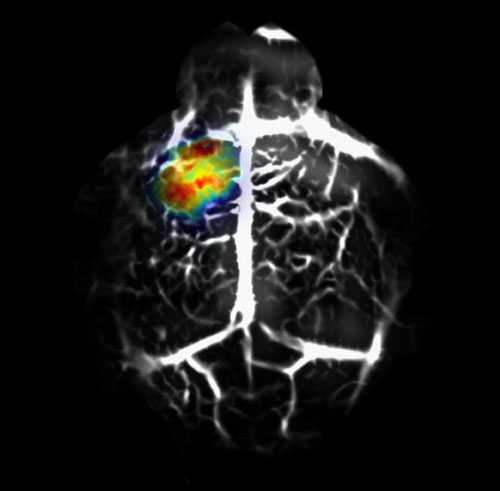
| Deep-tissue in vivo photoacoustic genetic imaging of reversibly switchable bacterial phytochrome BphP1. The reversible switching of BphP1 enables differential photoacoustic imaging, which dramatically enhances the detection sensitivity of a BphP1-expressing tumor (shown in color scale) in the mouse brain. The overwhelming background signals from non-switchable blood vessels are shown in gray scale. (Image: Junjie Yao and Lihong Wang)
|
|
"Genetic encoding of the protein allows us to image and track targeted biological processes deep in tissue," Wang says. "The optical switching property of the protein enables new imaging capability."
|
|
The BphP1 protein has the ability to sense different types of light and shift its absorption properties accordingly. This feature allows the researchers to take two images of cancerous tissue using the two types of light -- in this case, red or near-infrared light -- and compare them to get a highly sensitive, high-resolution image of the cancer cells.
|
|
Using two embodiments of photoacoustic tomography, both developed in Wang's lab, that use a combination of light and sound to take an intensely close look at tissues at different length scales, the researchers first illuminated the protein expressed in the cancerous tissue with near-infrared light, causing it to shift its absorption. Then, they shined red light on the tissue, essentially "flipping the switch" of the protein so that it goes back to its original state. When they subtract the second image from the first, the blood signal and other unwanted "background" in the image are eliminated, so that the cancer cells and their metastases are clearly visible.
|
|
"This technique is extremely useful for cancer imaging," Yao says. "When we first look at the early-stage cancer, cancer tissue does not differ much from the background, healthy tissue. Because the abundant blood gives strong signals, the cancer cells don't stand out. Now, with this new technology, we can see cancer cells in a tiny bit of tissue when the cancer is small."
|
|
Previously, Yao says, the team could see only relatively late-stage cancer in tissue because of the very strong background signal from blood that overshadows the cancer cells. That forced them to wait until the tumor grew large enough that it accumulated enough cells to be visible.
|
|
Yao says the new technology has promise for future studies of cancer as well as for studies of heart tissue and immunotherapy for cancer.
|
|
"This technology provides a promising new tool to biologists for high-resolution, deep imaging of cancer with genetic specificity as well as for drug screening in living tissue," Wang says.
|