| Mar 27, 2013 |
Revolutionary nanotechnology burns dressing glows when it detects an infection
|
|
(Nanowerk News) Chemists at the University have developed a prototype medical dressing that detects the first signs of the lethal Toxic Shock Syndrome along with other burn wound infections and could potentially save the lives of children with serious burns.
|
|
Toxic Shock Syndrome (TSS) is a serious complication of burn infections and particularly dangerous in children under four due to their immature immune systems. Left untreated, a child with a relatively small burn who develops TSS can rapidly deteriorate within a few hours. If left untreated, fifty per cent of children with the full-blown disease can die.
|
|
Scientists at the University of Bath have been working with clinicians at the South West Paediatric Burns Centre at Frenchay Hospital in Bristol to create an advanced wound dressing that can detect key microbial pathogens including the bacteria which cause TSS.
|
|
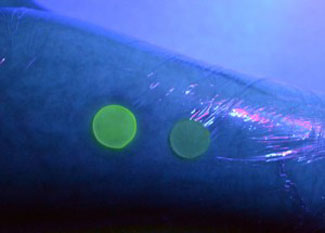
They have now developed a prototype dressing that releases dye from nanocapsules triggered by the presence of disease-causing pathogenic bacteria. The dye fluoresces under ultraviolet (UV) light, alerting healthcare professionals that the wound is infected.
|
|
The nanocapsules mimic skin cells in that they only break open when toxic bacteria are present, not responding to the harmless bacteria that normally live on healthy skin.
|
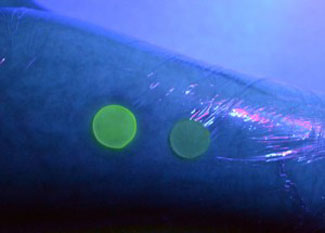 |
| The dressing glows under UV light when it detects an infection (left), but isn't affected by the bacteria normally found on healthy skin (right).
|
|
Dr Toby Jenkins, Reader in Biophysical Chemistry at Bath, is leading the project. He explained: “Around 5,000 children a year in England and Wales are hospitalised or treated in hospital with serious burns, mostly scalds caused by tea and coffee.
|
|
“The big problem for clinicians is the fast diagnosis of infection. Current methods take between 24 and 48 hours to get an answer as to whether the wound is infected.
|
|
“However our burns dressing gives a simple colour change under UV light if a pathogenic, disease-causing bacteria is present in the burn, meaning clinicians can be alerted quickly to a potential infection.”
|
|
Dr Amber Young, Consultant Paediatric Anaesthetist at the South West Paediatric Burns Centre at Frenchay Hospital and Paediatric Clinical Lead South West UK Burn Care Network, is the clinical consultant on the project. She said: “At the moment when a child with a small burn develops a high temperature we have no easy way of knowing if the child has a serious bacterial infection, or simply a cough or cold.
|
|
“We currently have to remove the dressing to test for infection, which may result in slower healing and potentially life-long scarring, and is very distressing for the child. This new dressing will mean we will be able to detect the early signs of infection so we can diagnose and treat the child quickly.
|
|
“It could make a real difference to the lives of many thousands of children.”
|
|
The prototype has been tested on skin samples in the lab and is currently being optimised for stability and shelf-life. The researchers expect to start safety trials on healthy human volunteers in four years.
|