| Posted: Oct 31, 2007 | |
On beating cancer (with nanotechnology) |
|
| (Nanowerk Spotlight) Cancer is an enormous socio-economic problem. According to the National Cancer Institute (NCI), it is estimated that in 2007 there will be over 1.4 million new cases of cancer (of any type) and over 550,000 deaths from cancer in the United States (you can download a detailed Cancer Statistics 2007 Presentation) from the American Cancer Society. | |
| This makes cancer the second deadliest disease category, after heart diseases. But while the mortality rates for heart diseases have dropped by more than half from 1950 to 2004, and other major disease categories show similar trends, cancer death rates have stayed pretty much the same. Shocking but true, if you are a male living in the U.S., your lifetime probability of developing some type of cancer is 1 in 2. | |
| If you are female, your probability is 1 in 3. Equally dismal are the economic cost associated with this disease: The amount of direct cancer-related costs (treatment, care and rehabilitation) have reached $74 billion in the U.S. in 2005, and growing fast, while the overall economic costs (including loss of economic output due to days off and premature death) are estimated to be over $200 billion per year (2005 data). | |
| This Nanowerk Spotlight will discuss existing and new approaches to fight cancer and their limitations. The goal is to stimulate readers to support and participate in interdisciplinary research and teaching efforts toward relieving suffering and death due to cancer. Fighting cancer involves three phases: (i) detection, (ii) treatment, and (iii) monitoring. Success depends on matching science to the actual practical needs. | |
| We'll take a look at - in particular nanotechnology - efforts underway in the direction of these three phases and comment on some of the practical problems encountered fighting cancer. We also speculate about some unconventional research that might be successful fighting cancer in the future. | |
| Detecting Cancer | |
| Detection at the earliest stage provides the greatest chance of survival. Cancer has a logarithmic growth rate. A one cubic centimeter size tumor may have 40-50 cell divisions and typically we don’t see 80% of the life of a tumor. Detection can be done using a number of techniques – including standard immunoassays and biopsies. | |
| Nanotechnology offers new detection approaches such as targeted contrast agents, nanoscale cantilevers coated with antibodies against tumor markers, and magnetic nanoparticles coated with DNA labeling. But the problem is daunting because there are over 50 common types of cancer and in practice it is difficult to ask people to come to the clinic on a regular basis for cancer screening. Early detection may require identifying a single cancer cell in 3,000 normal cells. Amplification strategies and simple tests are needed. Physicians ideally would like a quick digital readout sensor that can tell cancer is there or not. | |
| Nanotube electronic biosensors are being developed that might help in the detection of cancer (further reading: Edited Book to be published in 2008: Nanomedicine Science and Engineering; Mark J. Schulz, Vesselin N. Shanov, YeoHeung Yun, (Artech House Publishers, "Engineering in Medicine & Biology" book series); and: YeoHeung Yun, Zhongyun Dong, Vesselin Shanov, William R. Heineman, H. Brian Halsall, Amit Bhattacharya, Laura Conforti, Raj K. Narayan, William S. Ball, and Mark J. Schulz: Carbon Nanotube Electrodes and Biosensors, NanoToday Online Journal; to be published in Dec. 2007, vol. 2, no. 6). | |
| Treatment | |
| Cancer treatment typically involves chemotherapy, radiotherapy, or surgery, and – depending on the stage of the disease – often is unsuccessful. Many new techniques to treat cancer are under development. Bioactive immune stimulation and attacking integrin expressing vasculature using nanoparticles with gas bubbles that can explode by ultrasound are two novel approaches. Delivery of drugs to the cancer site using nanoparticles is currently being widely investigated. | |
| Nanoparticles such as multifunctional polymers, gold nanoshells, and carbon nanotubes are also being used as contrast agents to identify cancer, deliver drugs, and to ablate cancer cells. Nanoparticle devices hold great promise because they can treat cancer locally, potentially without harming the rest of the body. Based on presentations at the 3rd annual meeting of the American Academy of Nanomedicine, development of nanoparticles against cancer is an intense area of nanomedicine research. | |
| Devices such as micro-cantilever sensors and tiny cameras that can operate in the body are also under development. Micro and nano devices hold promise because they can go throughout the body to find cancer. Tumors have certain general characteristics that might be weak links that allow developing simpler generic techniques to treat cancer. The generic techniques might be successful especially where cancer cells become resistant to medication. | |
| The difficulty of treating cancer is shown by testing using mouse models. Artificially induced cancer can be cured in mice using several new techniques, but in humans the therapies are often not as effective. Some characteristics of cancer that might be taken advantage of to develop simple therapies are high pressure in the tumor (which is why drug delivery is difficult), high pH levels, elevated temperature, different elasticity of the tissue, and new vasculature and blood supply. | |
| Nanodevices are being designed conceptually at the University of Cincinnati's Smart Structures Bio-Nanotechnology Laboratory that focus on identifying and destroying cancer cells based on the material properties of the cells, rather than on complex cancer biology. Simple tools are needed when cancer cells become resistant to drugs. Biosensors to measure physiological variables such as pressure, temperature, pH, cell membrane and neural potentials, and chemical and inorganic ion concentrations are considered feasible to develop and may identify and locate cancer without the need for complex biochemistry. | |
| Responsive biosensors may also react to the cancer by coupling to RF signals to ablate cancer cells, or release drugs, or radiation, or to block the vasculature. Miniature sensors that operate in the body could be developed based on electro-mechanical-systems built from nanoparticles such as nanotubes, nanowires, nanobelts, and nanosphere chains that have smart materials properties including sensing, actuation, and power generation. | |
| Monitoring for the Recurrence of Cancer | |
| Monitoring involves detection of the recurrence and spread of cancer after initial treatment and remission. Physicians would be helped by an easy to use sensor that can perform a quick check for cancer. Monitoring prostate cancer, for instance, would be one important application for the sensor. In 2005 in the United States, there were an estimated 230,000 new cases of prostate cancer and 30,000 deaths due to prostate cancer. Most prostate cancer deaths are caused by metastases that are resistant to conventional therapies. | |
| As detection techniques improve, an increasing number of patients are diagnosed with localized prostate cancer, whereas the number of patients with disseminated disease is on the decline. But in many patients, metastasis occurs prior to initial diagnosis, and hence eradication of primary tumors by either surgery or radiation therapy is not curative. Currently, there is no technology to differentiate patients with disseminated disease from others diagnosed as having clinically localized prostate cancer. An electronic needle sensor would be useful to predict the metastatic potential of diagnosed prostate tumors which would improve the efficiency of point-of-care and clinical testing, and may provide near real-time diagnostics during surgery. | |
| Detection of cancer cells in blood is another approach that would provide information about the metastatic potential of the cancer, and therefore clinical outcomes. The treatment for metastasis is much more severe to the patient than the treatment for no metastasis, and avoiding the former treatment is a significant benefit to the patient. A small needle biosensor inserted directly into the blood or a tumor might provide the information needed to differentiate between metastatic and non-metastatic cancer. A cell sensor would identify the circulation of cancer cells in the blood related to prostate cancer in its early stages when this critical information is needed to determine the most efficacious course of treatment. | |
| Initial testing of a cell biosensor described in a recent paper in Nanotechnology ("Electrochemical impedance measurement of prostate cancer cells using carbon nanotube array electrodes in a microfluidic channel") showed that a nanotube electrode can characterize different solutions of LNCaP prostate cancer cells. | |
| The testing suggests that a cell-based biosensor may be used for metastasis detection. Further development of this sensor is needed to discriminate cancer cells from other types of cells. Selectivity of cells will be attempted using gold functionalized nanotube array electrodes with bio conjugation using antibodies, or special receptors. It is hoped this electronic sensor can detect different types of cancer cells in the blood in a quick electronic measurement. Once cancer has occurred, we usually know what type of cancer to look for to check for metastasis. In this case, the sensor can be designed specifically to detect that type of cancer cell using antibodies. | |
| Responsive Materials and Devices | |
| The nanotechnology approaches that are being taken toward beating cancer that are described above are considered to have a likelihood of success for many applications. On the other hand, some cancers are drug resistant or mutate after initial therapy and treatment is mostly ineffective. This is where drastic approaches and new medicine are needed to combat cancer. | |
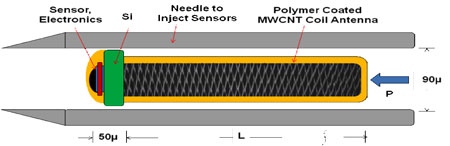
| A revolutionary approach is to develop responsive materials and devices to go inside the body to combat cancer. Responsive materials have an intrinsic ability to sense and respond to external stimuli. Examples are multi-wall carbon nanotubes that act as bearings and also telescope and change electrical resistance, carbon nanotubes that strain based on electrochemical bond expansion, nanowires that generate power, and piezoelectric nanobelts that bend. Devices that could be fabricated from responsive materials include inductors and solenoids built from nanowires and coiled nanotubes, electronic components such as transistors, antennas, and wires, and simple motors and pumps. Three factors must be considered to develop responsive materials as medical devices for in vivo applications: (i) delivery; (ii) monitoring; and (iii) retrieval of the devices. It is conceivable to develop a sub-millimeter diameter sensor device with a mm long antenna tail: | |
 |
|
| Concept in-body responsive device: Injectable wireless tumor sensor. (Image: Prof. Schulz) | |
| This device could be delivered and injected into the body to receive, sense, and transmit limited information about physiological variables that could identify a tumor. Ion flux propulsion might provide mobility of the device. On a smaller scale, micron size electronic responsive particles could circulate in the blood stream and receive wireless signals to release drugs, or heat to kill cells, or vibrate to clean arteries and report their location as the sensor circulates in the body. | |
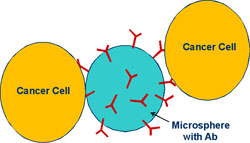
| A still simpler responsive-material approach is to use micron size particles functionalized with antibodies to capture cancer cells in the blood, or the particles could sample fluids from certain areas of the body based on capillarity: | |
 |
|
| Concept in-body responsive device: Circulating magnetic microsphere with antibodies to capture cancer cells for examination outside the body. (Image: Prof. Schulz) | |
| The sensor or functionalized particles would be magnetically removed from the blood and analyzed to identify metastasis potential. Going further, mobile microscopic robots using nanomanipulators built using nanowire solenoids would do surgery and repairs in the body. Methods of retrieval of devices using surgery or other ways or the effects of leaving the device in the body are practical problems that must be solved. Biocompatibility and biological integration may be solved using coatings or by responsive sensors that can self-clean their electrodes. | |
| Conclusion | |
| Looking ahead, it appears that eradicating cancer will require integrating basic science, engineering, and medical knowledge to develop a toolbox of general methods to treat different cancers. Also needed is development of the most advanced technologies and devices ever conceived by mankind that will operate in the body to treat disease at the cellular and molecular levels. Development of this new medicine will be a fantastic voyage that we are literally betting our lives on. | |
| By Mark J. Schulz, YeoHeung Yun, Zhongyun Dong, Vesselin N. Shanov, and Michael Berger. Copyright Nanowerk LLC | |
|
Become a Spotlight guest author! Join our large and growing group of guest contributors. Have you just published a scientific paper or have other exciting developments to share with the nanotechnology community? Here is how to publish on nanowerk.com. |
|
