| Posted: May 01, 2014 | |
Nanoparticle trafficking in the central nervous system |
|
| (Nanowerk Spotlight) Nanotechnology's growing significance in dealing with brain disorders is exemplified by the nanomedicine-enabled approaches that are being developed for early detection and accurate diagnosis of Alzheimer's, its therapeutic treatment, and prevention (read more: "Fighting Alzheimer's disease with nanotechnology"). | |
| Prevention and treatment of neurological disorders in humans – such as for example Parkison’s disease, Alzheimer’s disease, Huntington disease, multiple sclerosis and brain tumors – necessitate delivery of therapeutic or neuroprotective agents across the so-called blood-brain barrier (BBB) into the brain. This barrier, a tight seal of endothelial cells that lines the blood vessels in the brain, is a physiological checkpoint that selectively allows the entry of certain molecules from blood circulation into the brain. | |
| The scarcity of techniques for brain-specific delivery of therapeutic molecules using non-invasive approaches has led researchers to increasingly explore the promising potential of nanotechnology – by means of surface-engineered nanocarriers – toward the diagnosis and treatment of diseases/disorders incurable with present techniques (read more: "Crossing the blood-brain barrier with nanotechnology"). | |
 |
|
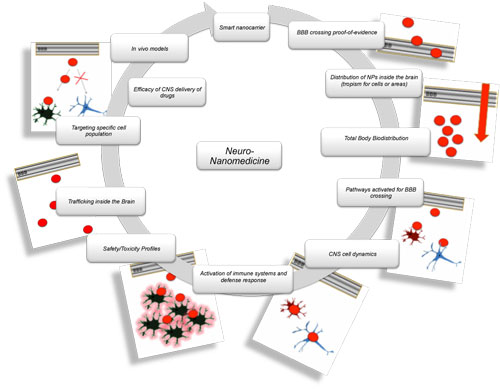
| Schematic representation of development of nanomedicines for Central Nervous System targeting. Each task represents a pivotal aspect to be addressed by both academic and industrial research programs on neuro-nanomedicine. (Image: Dr. Tosi, University of Modena and Reggio Emilia) (click image to enlarge) | |
Nanoparticles for drug delivery to the central nervous system |
|
| A recent example of these efforts is the research by German and Italian scientists to analyze the intra- and intercellular transport and fate of novel nanoparticles for drug delivery to the central nervous system (CNS). | |
| "We investigated the possible mechanisms of a cell-to-cell transport of highly biocompatible polymer (poly-lactide-co-glycolide, PLGA) nanoparticles modified with a glycopeptide (g7), termed g7-NP – already demonstrated to be able to cross the BBB after in vivo administration in rodents – in a living mouse brain," Giovanni Tosi, PhD, a researcher belonging to the Center for Traditional and Innovative Pharmaceutical Technology (Te.Far.T.I.), headed by Prof. Vandelli and Prof. Forni, at the Department of Life Sciences at the University of Modena and Reggio Emilia, tells Nanowerk. | |
| The researchers published their findings in two papers in the Journal of Controlled Release: "Insight on the fate of CNS-targeted nanoparticles. Part I: Rab5-dependent cell-specific uptake and distribution" and "Insight on the fate of CNS-targeted nanoparticles. Part II: Intercellular neuronal cell-to-cell transport". | |
| Both papers give several insights regarding the dose/time dependent accumulation of nanoparticles in the brain, their regional distribution and cell tropisms, uptake mechanisms, inter- and intra-cellular transport, and existing in vivo/in vitro correlations. | |
| According to Tosi, the principal novelty of the study consists in the detailed assessment of the brain cell subpopulations that uptake g7-NPs after a systemic administration, i.e., mimicking a route of administration that may be used in human patients. | |
Nanotechnology for neurodegenerative disorders |
|
| "The principal result of our study is the demonstration of a strong tropism of g7-NPs for cortical interneurons," he says. "This is of main translational relevance since GABAergic interneuronal systems have been shown to play a pathogenic role in several neuropsychiatric diseases, including seizures, neuropathic pain, major psychosis and anxiety. Therefore, g7-NPs can be proposed as promising carriers to deliver therapeutic agents for the treatment of major neuropsychiatric and neurodegenerative disorders." | |
| Tosi notes that the application of nanomedicine to difficult-to-treat pathologies shows potential advantages with respect to other kinds of therapeutic strategies. "In fact, both the feasibility of nanocarriers and the possibility of engineering the surface of these systems allow specific and selective drug delivery and targeting." | |
| Nanoparticles and liposomes have been currently investigated during in vitro and in vivo neuroscience experiments showing important results in terms of their ability in BBB crossing and CNS targeting. | |
| "Notwithstanding the stimulating results achieved, the development of a nanotechnology-based neurological medicine is a long way off," says Tosi. "Many critical aspects, regarding the complexity of both the nanotechnology area – preparation, engineering, characterization, safety – and the disease-related pathophysiology – BBB state, altered cellular metabolism, cell-to-cell dynamics – remain to be solved." | |
| "Despite these difficulties" he concludes, "we are optimistic that the solution of these problems will come soon when neuroscientists and experts of nanotechnology will combine their efforts to create a network of laboratories dedicated to this subject." | |
 By
Michael
Berger
– Michael is author of three books by the Royal Society of Chemistry:
Nano-Society: Pushing the Boundaries of Technology,
Nanotechnology: The Future is Tiny, and
Nanoengineering: The Skills and Tools Making Technology Invisible
Copyright ©
Nanowerk LLC
By
Michael
Berger
– Michael is author of three books by the Royal Society of Chemistry:
Nano-Society: Pushing the Boundaries of Technology,
Nanotechnology: The Future is Tiny, and
Nanoengineering: The Skills and Tools Making Technology Invisible
Copyright ©
Nanowerk LLC
|
|
|
Become a Spotlight guest author! Join our large and growing group of guest contributors. Have you just published a scientific paper or have other exciting developments to share with the nanotechnology community? Here is how to publish on nanowerk.com. |
|
