Nanotechnology's role in HIV AIDS treatment
HIV continues to be a major global public health issue, having claimed about 40 million lives so far. According to the World Health Organization (WHO), in 2021, 650 000 people died from HIV-related causes and 1.5 million people acquired HIV. There were an estimated 38.4 million people living with HIV at the end of 2021, two thirds of whom are in the African Region.
A cure for HIV/AIDS has been elusive in almost 30 years of research. Early treatments focused on antiretroviral drugs that were effective only to a certain degree. However, it was the advent of a class of drugs known as protease inhibitors and the introduction of triple-drug therapy in the mid-1990s that revolutionized HIV/AIDS treatment. This launched the era of highly active antiretroviral therapy (HAART), where a combination of three or more different classes of antiretroviral drugs are administered simultaneously.
However, some HAART regimens have serious side effects and, in all cases, HAART has to be taken for a lifetime, with daily dosing of one or more pills. Some patients also develop resistance to certain combinations of drugs, resulting in failure of the treatment. The absence of complete cure under current treatment underscores the great need for continued efforts in seeking innovative approaches for treatment of HIV/AIDS.
To address this issue, researchers have been exploring the use of nanotechnology in the treatment of HIV. Nanosystems offer several advantages over traditional treatments, including increased bioavailability, solubility, stability, and the ability to target specific cells. This can lead to more effective treatments with fewer side effects, making them more accessible and affordable to those who need them.
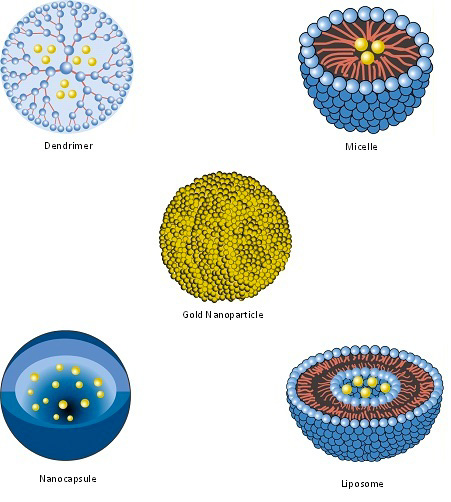
Common nanotechnology-based systems for HIV treatment include liposomes, nanoparticles, niosomes, polymeric micelles, and dendrimers. For example, traditionally, the antiviral efficacy of classic cocktail therapy is significantly limited by the distinct pharmacokinetic profiles of partner therapeutics that lead to inconsistent in vivo bio-distribution. In one research study, scientists developed a new cocktail-like drug delivery vehicle using biodegradable polymeric nanoparticles encapsulating non-nucleoside reverse transcriptase inhibitor, surface-conjugated with HIV-1 fusion inhibitor, and aiming to achieve enhanced cellular uptake, improved antiviral activity and prolonged blood circulation time.
Research over the past years has shown that nanotechnology approaches can enhance current treatment as well as advance new therapeutic strategies, such as gene therapy and immunotherapy. Moreover, some nanomaterials have therapeutic effects by themselves.
Nanotechnology can also play a major role in preventive strategies for developing vaccines and microbicides.
Main nanotechnology-based systems explored for HIV therapeutics are liposomes, nanoparticles, niosomes, polymeric micelles, and dendrimers.
Liposomes
Liposomes are microscopic vesicles consisting of one or more phospholipid bilayers which usually surround an aqueous core. Liposomes are having size between 25 nm and several microns.
When liposomes enter in the human body, they are recognized as foreign bodies and easily taken up by the mononuclear phagocytic cells. HIV is present in mononuclear phagocytic cells of infected patient, so liposomes represent suitable carriers for targeting anti-HIV drugs to the infected cells. Thus, liposomes can improve the efficacy of anti-HIV drugs and reduce their side effects.
Nanoparticles
Nanoparticles are solid colloidal particles having size range 10 1000 nm. They are capable to target drug to specified sites in the body along with its sustained release depending upon their colloidal size and polymeric composition.
Three types of nanoparticles are mainly employed for anti-HIV therapeutics: Polymeric nanoparticles; solid lipid nanoparticles and nanostructured lipid carriers; and inorganic nanoparticles.
Nanoparticles are also explored for improvement of formulation and efficacy of drugs with physico-chemical drawbacks like poor stability and solubility. They are being increasingly investigated for targeted delivery of ARVs to HIV-infected cells and to achieve sustained drug-release kinetics.
Drug encapsulation into such systems may provide improved efficacy, decreased drug resistance, the reduction in dosage, a decrease in systemic toxicity, and side effects, and an improvement in patient compliance.
Niosomes
Niosomes are also known as nonionic surfactant vesicles. They are formed from self-assembly of hydrated synthetic nonionic surfactant monomers and are capable of entrapping a variety of drugs. Niosomes have been evaluated as an alternative to liposome.
Polymeric micelles
Polymeric micelles are nanostructures of less than 100 nm diameter that have been utilized for improving aqueous solubility, intestinal permeability, and disease site targeting of several drug molecules. Polymeric micelles are composed of block polymers and are having a coreshell arrangement – a core (hydrophobic block) and a shell (hydrophilic block) – that is similar to surfactant-based micelles.
Dendrimers
A dendrimer is a polymeric nanostructure (<100 nm) built around a core unit. There are several branching units around the core units in a layer-by-layer fashion which defines the growth, size, and the microenvironment within the dendrimer.
Dendrimers are composed of a large number of smaller units known as dendrons. Dendrons are formed after removal of core units and can be divided into (empty) core, the interior (branching units), and the periphery (end groups). The empty space lying inside the dendrons can be used for the entrapment of drug molecules for solubilization, controlled release, targeting, or protection from surrounding degrading environment.
Antiretroviral therapy
There are more than 25 anti-retroviral drugs approved for use in HIV-infected individuals, from at least six mechanistic classes, which include the nucleoside/nucleotide reverse transcriptase
inhibitors, non-nucleoside reverse transcriptase inhibitors, protease inhibitors, fusion inhibitors, CCR5 antagonists and integrase strand transfer inhibitors (source).
However, because they are unable to eradicate viral reservoirs, none of these drugs are curative and lifelong treatment with durable viral suppression is currently the goal of therapy. There are, however, serious challenges to long term suppression of viral replication, which include non-adherence, drug toxicity, drug interactions and the inevitable appearance of drug resistant mutations.
The convergence of pharmacology and nanotechnology seeks to address some of these issues by creating or enabling some of the following elements:
Gene therapy
RNA-based therapies are an attractive prospect for the treatment, not only of HIV, but of a wide variety of other infectious and non-infectious diseases. Strategies include ribozymes, antisense RNAs, RNA aptamers, RNA decoys, human ribonuclease P, modified small nuclear RNA and small interfering RNAs.
Numerous methods for non-viral delivery of therapeutic DNA and RNA have been explored. In particular, nanosized drug carrier systems have been developed that may address many of the issues related to nucleic acid delivery: Improved safety (due to biodegradability and rapid clearance by the reticuloendothelial system), targeted delivery and controlled release, improved uptake by overcoming electrostatic repulsion between negatively charged RNA or DNA and cell membranes, improved stability in physiological fluids and protection from degradation.
An overview of recent research results
Diagnostics
Therapeutics
Opiate abuse is a significant risk factor for HIV infection, and in combination they can have a devastating effect on the brain. Scientists are studying new therapies that can short-circuit HIV infection and mitigate the damaging effects that opiate addiction has on the central nervous system. (Nanotechnology based gene editing to eradicate HIV brain reservoir in drug abusers).
Further reading
"Nanotechnology: A magic bullet for HIV AIDS treatment", Artificial Cells, Nanomedicine, and Biotechnology
