| Posted: Nov 29, 2016 |
Researchers load nanocarriers to deliver chemotherapy drugs and imaging molecules to tumors
(Nanowerk News) A conundrum of cancer is the tumor's ability to use our bodies as human shields to deflect treatment. Tumors grow among normal tissues and organs, often giving doctors few options but to damage, poison or remove healthy parts of our body in attempts to beat back the cancer with surgery, chemotherapy or radiation.
|
|
But in a paper published Sept. 27 in the journal Small ("Preloading of Hydrophobic Anticancer Drug into Multifunctional Nanocarrier for Multimodal Imaging, NIR-Responsive Drug Release, and Synergistic Therapy"), scientists at the University of Washington describe a new system to encase chemotherapy drugs within tiny, synthetic "nanocarrier" packages, which could be injected into patients and disassembled at the tumor site to release their toxic cargo.
|
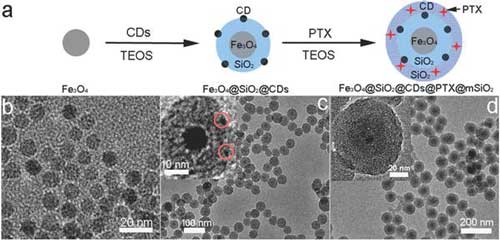 |
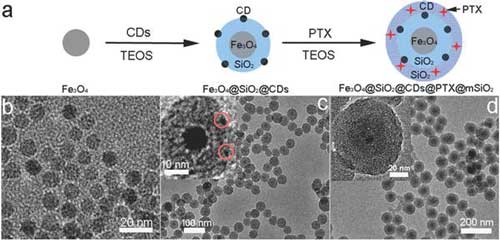
| Zhang's group created this nanocarrier using a "load during assembly" approach, shown along the top. Images b, c and d are microscopic views of the nanocarriers at each major step of the assembly and loading process. (Image: Miqin Zhang) (click on image to enlarge)
|
|
The group, led by UW professor of materials science and engineering Miqin Zhang, is not the first to work on nanocarriers. But the nanocarrier package developed by Zhang's team is a hybrid of synthetic materials, which gives the nanocarrier the unique ability to ferry not just drugs, but also tiny fluorescent or magnetic particles to stain the tumor and make it visible to surgeons.
|
|
"Our nanocarrier system is really a hybrid addressing two needs -- drug delivery and tumor imaging," said Zhang, who is senior author on the paper. "First, this nanocarrier can deliver chemotherapy drugs and release them in the tumor area, which spares healthy tissue from toxic side effects. Second, we load the nanocarrier with materials to help doctors visualize the tumor, either using a microscope or by MRI scan."
|
|
Their hybrid nanocarrier builds on years of research into the types of synthetic materials that could package drugs for delivery into a specific part of a patient's body. In previous attempts, scientists would often first try make an empty nanocarrier out of a synthetic material. Once assembled, they would load the nanocarrier with a therapeutic drug. But this approach was inefficient, and carried a high risk of damaging the fragile drugs and rendering them ineffective.
|
|
"Most chemotherapy drugs have complex structures -- essentially, they're very fragile -- and they do no good if they are broken by the time they reach the tumor," said Zhang.
|
|
Zhang's team worked around this problem by designing a nanocarrier that could be assembled and loaded simultaneously. Their approach is akin to laying cargo within a shipping container even as the container's walls, floor and roof are being assembled and bolted together.
|
|
This "load during assembly" technique also let Zhang's team incorporate multiple chemical components into the nanocarrier's structure, which could help hold cargo in place and make the tumor easy to image in clinical settings.
|
|
Their nanocarrier sports a core of iron oxide, which provides structure but can also be used as an imaging agent in MRI scans. A shell of silica surrounds the core, and was designed to efficiently stack the chemotherapy drug paclitaxel. They also included space in the nanocarrier for carbon dots, tiny particles that can "stain" tissue and make it easier to see under a microscope, helping doctors resolve the boundaries between cancerous and healthy tissue for further treatment or surgery. The intensity of many imaging agents fades over time, but Zhang said this nanocarrier can provide sustained imaging for months.
|
|
Yet despite holding so much cargo, the fully loaded nanocarriers are less than the thickness of a sheet of flimsy notebook paper.
|
|
The silica shell keeps the nanocarriers watertight. In addition, they do not interfere with healthy tissue, as Zhang's team showed by injecting healthy mice with empty nanocarriers or nanocarriers loaded with drug cargo. Five days after injection, they checked vital organs in the mice for evidence of toxicity and found none.
|
|
"This would indicate that the nanocarriers themselves do not trigger an adverse reaction in the body, and that the loaded nanocarriers are keeping their toxic cargo shielded from the body," said Zhang.
|
|
The UW team also designed the nanocarriers to be easily disassembled once they reached a desired location. Gentle heating from low-level infrared light was sufficient to make the nanocarriers break apart and disgorge their cargo, which is something doctors could apply to the tumor site during treatment.
|
|
As their final test of the nanocarrier effectiveness, Zhang's team turned to mice with a form of transmissible cancer. Mice that they injected with empty nanocarriers showed no reduction in tumor size. But tumors shrank significantly in mice injected with nanocarriers that were loaded with paclitaxel. They saw a similar affect on human cancer cells cultured and tested in the lab.
|
|
"These results show that the nanocarriers can deliver their cargo intact to the tumor site," said Zhang. "And while we designed this nanocarrier specifically to accommodate paclitaxel, it is possible to adjust this technique for other drugs."
|
|
There are still mountains to climb before this technology is proven safe and effective for humans. But Zhang hopes her team's approach and promising results will accelerate the ascent.
|