| Mar 02, 2012 |
Finding cancer cells in blood
|
|
(Nanowerk News) Even in the early stages of cancer, individual cancer cells can be found in the blood. Certain subsets of these circulating tumor cells can cause metastasis. In cases of breast cancer, it is known that these cells can differ from the original tumor cells, which allows them to survive treatment to cause later recurrence. It could thus be quite informative to detect these cells in the blood and examine them more closely.
|
|
In the journal Angewandte Chemie ("Sensitive and High-Throughput Isolation of Rare Cells from Peripheral Blood with Ensemble-Decision Aliquot Ranking"), researchers at the University of Washington (Seattle, USA) describe a new chip-based method that allows for the detection and isolation of tiny concentrations of such cells in blood.
|
 |
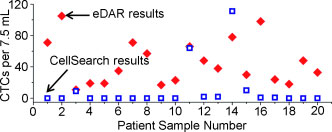
| Enrichment of cells: An approach called ensemble-decision aliquot ranking (eDAR) for isolating rare cells from peripheral blood is described. The eDAR process has a recovery of over 93% (number of runs n=9) with a zero false positive rate (n=8) and provides direct easy access to individual isolated live cells for downstream single-cell manipulation and analysis (CTCs=circulating tumor cells).
|
|
The detection of circulating tumor cells is a difficult challenge because it requires the detection of quantities as low as one to ten cells per milliliter of blood—in the presence of large numbers of red blood cells and other cells. Conventional methods cannot manage this, but scientists led by Daniel T. Chiu have now developed a microfluidic system that allows for the analysis of 1 mL of blood within 20 minutes. The secret of their success is to virtually divide the sample into aliquots (portions) and to search these for the presence or absence of the desired cell types.
|
|
The blood is initially marked with fluorescent markers that specifically bind to the desired tumor cells. The sample is then passed through a system of microchannels, where it passes through a zone that is irradiated by a laser. The size of this zone determines the volume of the virtual aliquot; 2 nanoliters was found to work well. The laser causes the marker to fluoresce if marked cells are present. It can thus be determined whether or not an aliquot contains one (or more) of the desired cells. If the aliquot fluoresces, it is automatically pumped into a different channel than the fractions that do not fluoresce. The positive aliquots enter a filtration chamber. Red blood cells and the majority of blood cells pass through the filter; tumor cells are larger and are trapped. They can be counted on the filter, examined by microscope, or removed by micropipette for further examination. By using a second marker, certain subpopulations, such as tumor stem cells, can be identified.
|
|
Experiments with blood containing a known number of breast cancer cells yielded a recovery rate of 93 % and a false positive rate of zero. Real blood samples from patients were also examined and the results compared with those from a clinically established system. The new microfluidic system proved to be significantly more sensitive. This new procedure has potential for monitoring treatment, aftercare, and the early detection of cancer.
|