| May 15, 2012 |
Nanoparticle delivery system for gene therapy may help treat arthritis
|
|
(Nanowerk News) A DNA-covered submicroscopic bead used to deliver genes or drugs directly into cells to treat disease appears to have therapeutic value just by showing up, researchers report.
|
|
Within a few hours of injecting empty-handed DNA nanoparticles, Georgia Health Sciences University researchers were surprised to see increased expression of an enzyme that calms the immune response.
|
|
In an animal model of rheumatoid arthritis, the enhanced expression of indoleomine 2,3 dioxygenase, or IDO, significantly reduced the hallmark limb joint swelling and inflammation of this debilitating autoimmune disease, researchers report in the study featured on the cover of The Journal of Immunology ("Engineering DNA Nanoparticles as Immunomodulatory Reagents that Activate Regulatory T Cells").
|
|
"It's like pouring water on a fire," said Dr. Andrew L. Mellor, Director of the GHSU's Medical College of Georgia Immunotherapy Center and the study's corresponding author. "The fire is burning down the house, which in this case is the tissue normally required for your joints to work smoothly," Mellor said of the immune system's inexplicable attack on bone-cushioning cartilage. "When IDO levels are high, there is more water to control the fire."
|
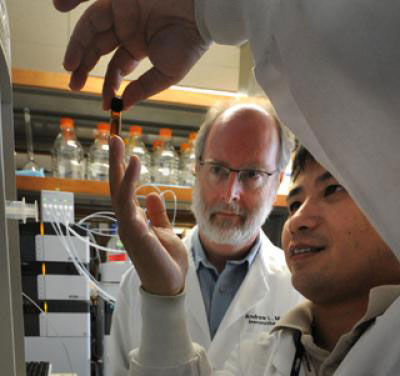 |
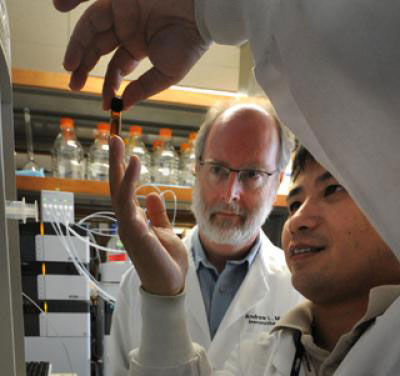
| Drs. Andrew L. Mellor and Lei Huang at Georgia Health Sciences University have shown a system called DNA nanoparticles, used to deliver genes or drugs directly into cells to treat a variety of diseases, may help arthritis without delivering anything.
|
|
Several delivery systems are used for gene therapy, which is used to treat conditions including cancer, HIV infection and Parkinson's disease. The new findings suggest the DNA nanoparticle technique has value as well for autoimmune diseases such as arthritis, type 1 diabetes and lupus. "We want to induce IDO because it protects healthy tissue from destruction by the immune system," Mellor said.
|
|
The researchers were exploring IDO's autoimmune treatment potential by inserting the human IDO gene into DNA nanoparticles. They hoped to enhance IDO expression in their arthritis model when Dr. Lei Huang, Assistant Research Scientist and the paper's first author, serendipitously found that the DNA nanoparticle itself produced the desired result. Exactly how and why is still being pursued. Early evidence suggests that immune cells called phagocytes, white blood cells that gobble up undesirables like bacteria and dying cells, start making more IDO in response to the DNA nanoparticle's arrival. "Phagocytes eat it and respond quickly to it and the effect we measure is IDO," Mellor said.
|
|
Dr. Tracy L. McGaha, GHSU immunologist and a co-author on the current study, recently discovered that similar cells also prevented development of systemic lupus erythematosus in mice.
|
|
Follow-up studies include documenting all cells that respond by producing more IDO. GHSU researchers already are working with biopolymer experts at the Massachusetts Institute of Technology, the University of California, Berkeley and the Georgia Institute of Technology to identify the optimal polymer.
|
|
The polymer used in the study is not biodegradable so the researchers need one that will eventually safely degrade in the body. Ideally, they'd also like it to target specific cells, such as those near inflamed joints, to minimize any potential ill effects.
|
|
"It's like a bead and you wrap the DNA around it," Mellor said of the polymer. While the DNA does not have to carry anything to get the desired response in this case, DNA itself is essential to make cells express IDO. To ensure that IDO expression was responsible for the improvements, they also performed experiments in mice given an IDO inhibitor in their drinking water and in mice genetically altered to not express IDO. "Without access to the IDO pathway, the therapy no longer works," Mellor said.
|
|
Drs. Andrew Mellor and David Munn reported in 1998 in the journal Science that the fetus expresses IDO to help avoid rejection by the mother's immune system. Subsequent studies have shown tumors also use IDO for protection and clinical trials are studying the tumor-fighting potential of an IDO inhibitor. On the flip side, there is evidence that increasing IDO expression can protect transplanted organs and counter autoimmune disease.
|