| Mar 25, 2019 |
Traffic control of cells
|
|
(Nanowerk News) Cells in the human body can display remarkable differences in their behaviour depending on the mechanical properties of the tissue surrounding them. This is especially true for immune cells, which migrate through the body and are thus constantly exposed to tissues with different properties and must respond appropriately.
|
|
To enable investigation of how cells respond to dynamic changes in the stiffness of the extracellular environment, researchers from the Freiburg Signalling Research Clusters of Excellence BIOSS and CIBSS and the Cluster of Excellence livMatS joined forces to develop a hydrogel matrix whose stiffness can be reversibly tuned using light.
|
|
The study represents the first joint project between CIBSS and livMatS and is featured on the cover of the latest issue of Advanced Materials ("Phytochrome-Based Extracellular Matrix with Reversibly Tunable Mechanical Properties").
|
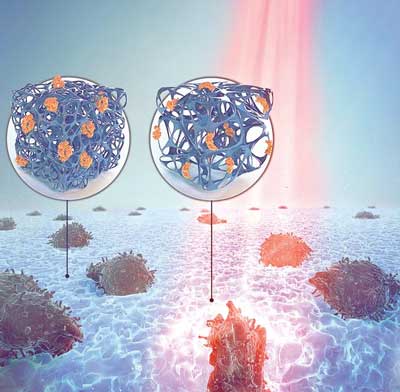 |
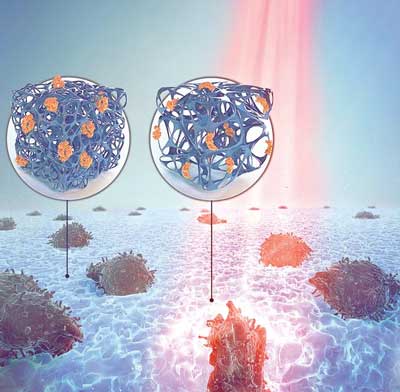
| The authors engineered a version of Cph1 with built-in binding sites for cells, and then used this modified photosensor to crosslink branched polyethylene glycol polymers. When the resulting hydrogel was exposed to red light, the Cph1 molecules bound one another and thereby increased the number of crosslinks and thus the stiffness of the matrix. (Image: Jo Richers)
|
|
In the field of optogenetics, light is used to precisely control cellular proteins and processes. Thus far, optogenetics has been primarily used to control events within cells.
|
|
“In many cases, tools that allow precise spatiotemporal control of the properties of the extracellular environment are lacking,” says Prof. Dr. Wilfried Weber, lead author of the study and member of the Speaker Team of CIBSS – the Centre for Integrative Biological Signalling Studies. “Our ongoing research shows that optogenetics-inspired approaches hold great promise for dissecting how cells respond to dynamic changes in their environment.”
|
|
The first step in creating a matrix whose stiffness can be reversibly tuned using light was to find an appropriate molecular switch. After reviewing their publicly available database of optogenetic switches, called OptoBase, the authors decided for the protein Cph1, a bacterial phytochrome which is sensitive to light: It binds to another Cph1 molecule when exposed to red light, and when exposed to far-red light the Cph1 dimers dissociate.
|
|
The authors engineered a version of Cph1 with built-in binding sites for cells, and then used this modified photosensor to crosslink branched polyethylene glycol polymers. When the resulting hydrogel was exposed to red light, the Cph1 molecules bound one another and thereby increased the number of crosslinks and thus the stiffness of the matrix.
|
|
In contrast, exposure to far-red light led to dissociation of Cph1 dimers and softening of the matrix. The group of Prof. Dr. Andreas Walther from the Cluster of Excellence livMatS – Living, Adaptive and Energy-autonomous Materials Systems was involved in the elucidation of the physical properties of the hydrogels – a critical parameter space for cellular migration – under different illumination conditions.
|
|
“This system is ideal for investigating how cells respond to dynamic changes in the mechanical properties of their environment,” explains first author Dr. Maximilian Hörner. “The properties of the material can be regulated within seconds in a fully reversible and finely tunable manner.”
|
|
In experiments analysing migration of T cells, a type of immune cell that can fight cancer, the authors demonstrated that only the softer parts of the matrix that were exposed to far-red light were permeable for migration of T cells.
|
|
“While we observed that tumour-fighting T cells fail to migrate through a stiff matrix, it is well known that tumour cells preferentially migrate through stiff tissues to initiate invasion and metastasis,” says group leader PD Dr. Susana Minguet, a collaborator on the study. “This tunable matrix recapitulates the dynamic environments immune cells face when migrating through healthy and tumour tissues and has the potential not only to explain the failure of some T cell-based cancer immunotherapies, but also to inspire improved therapeutic approaches.”
|