| Jan 28, 2021 | |
The revolutionary power of bio platforms - or why it took just 48 hours to develop the Covid-19 vaccine |
|
| (Nanowerk Spotlight) In the race to develop an effective COVID-19 vaccine there have been two distinct frontrunners among the dozens of companies involved: BioNTech and Moderna. | |
| Moderna designed the final version of its vaccine within 48 hours of analyzing the virus genome on January 11, 2020. Phase 1 trials began 60 days later (in comparison, it took 20 months of conventional vaccine development for the SARS vaccine to reach Phase 1). This vaccine was approved by the FDA on December 17, 2020 (the 11 months until approval were spent with testing and regulatory formalities). In a similar vein, BioNTech was able to rapidly redirect its mRNA technology platform from cancer to COVID-19 in a matter of weeks. | |
| And they did all that entirely on a computer using a digital copy of the virus (Chinese scientists had already sequenced its genome), without having access to the physical virus. Quite intriguingly, this means that a digital copy of the virus reached the U.S. and Europe before the actual virus emerged there. | |
| How is that possible? Well, the answer lies in the revolutionary nature of new industrialized biotechnology platforms that exploit breakthroughs in biological engineering and artificial intelligence. | |
| Rather than growing vaccines in bioreactors, a new generation of biotechnology companies designs instructions that the body then can use to produce its own therapy. | |
| These novel vaccines exploit the process by which cells build proteins from the information encoded in a single-stranded molecule called messenger RNA (mRNA). | |
| Once the COVID-19 vaccine enters a cell, the mRNA molecule tells it exactly how to build a piece of the SARS-CoV-2 virus. By exposing the body to this piece of virus induces its immune system to mount a response, thereby training the body to fight the real deal if it gets infected by SARS-CoV-2. | |
'The power of life' – what is mRNA and how does it work as a vaccine |
|
|
|
|
| Moderna has produced an informative video explaining the importance of mRNA science. | |
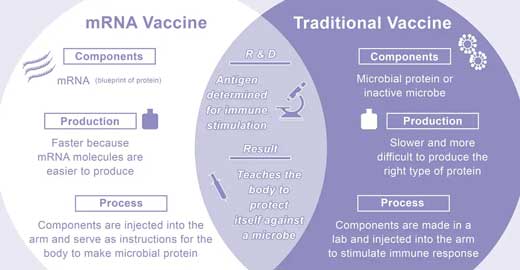
| Using mRNA as a vaccine – or any mRNA medicine, for that matter – is a fundamentally different approach than conventional vaccines. | |
| Traditional vaccines usually contain weakened or inactivated disease-causing organisms or pathogen proteins (antigens) to stimulate the body’s immune response. These conventional viral vaccines are manufactured in large bioreactors through a lengthy and cumbersome process – that can take many months – that involves numerous steps like preparation of the seed virus, fermentation, harvesting and purification. It also necessitates the handling of large volumes of live viruses grown in chicken eggs or mammalian cells. | |
| Take the example of the annual ritual of developing a vaccine against seasonal flu, which commonly takes about half a year from identification of the prevailing influenza virus strain to producing a vaccine. The candidate flu vaccine virus is grown for about three weeks to produce a hybrid virus, which is less dangerous and better able to grow in chicken eggs. The hybrid virus is then injected into a lot of fertilized eggs and incubated for several days to make more copies. Then the fluid containing the virus is harvested from eggs, the vaccine viruses are killed, and the viral proteins are purified over several days. | |
| mRNA vaccines eliminate pretty much all of this conventional manufacturing process. | |
| In contrast, mRNA vaccines are based on just sets of instructions – like a software code – that direct cells in the body to make proteins to prevent or fight disease. | |
| This makes mRNA vaccines very safe – they do not interact with the genome but just carry the information required for expression of the encoded protein. | |
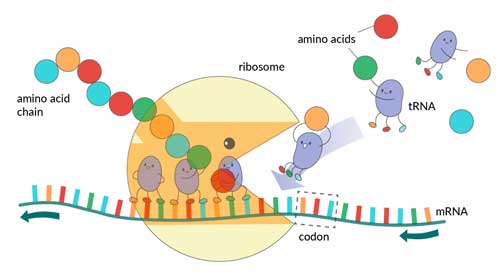
| The millions of proteins in our body are all made by piecing together different combinations of amino acids. And in this process mRNA plays a crucial role: It carries genetic code from DNA in the cell's nucleus (composed of four different building blocks – the nucleotides adenine, cytosine, guanine, and thymine) to the cell's protein-making machinery. These biological machines are called ribosomes and in some mammals every cell carries millions of them. Ribosomes read the mRNA and, based on the instructions (which contain hundreds or thousands of nucleotides linked in a unique order), synthesize a set of amino acids that are then folded into a specific protein. | |
 |
|
| Ribosomes read mRNA blueprints and piece together proteins, with the help of transfer RNA (tRNA) support workers that bring them the right amino acid each step of the way. (Image: Jovana Andrejevic) | |
| In short, without mRNA, the body wouldn’t be able to use the genetic code contained in DNA. Proteins would never get made. Basically, your body wouldn’t function. | |
Building mRNA vaccines for COVID-19 |
|
| Coronaviruses invade cells through surface molecules called spike proteins (named for the fact that they physically jut out from the rest of the virus), which take on different shapes in different coronaviruses. The SARS-CoV-2 specific spike protein is therefore a crucial antigen – i.e. a substance that induces the immune system to produce antibodies against it – that can be exploited for vaccine design. | |
| And this is how an mRNA vaccine against COVID-19 works: Once the virus genome is sequenced – that means it is available as a digital copy – researchers can design an mRNA sequence that encodes the blueprint for the virus spike protein. Once tested for efficacy and safety in clinical trials, the mRNA molecule can then be synthesized on an industrial scale in robotic factories. | |
| This mRNA molecule is wrapped with a lipid nanoparticle envelope, which protects it from degradation, and then directly delivered into cells. There, ribosomes get to work and read the mRNA as just any other blueprint – only this time they synthesize the spike protein. The finished spike proteins are then attached to the surface of cells where they are recognized by the immune system, eventually triggering the desired immune response against the virus. | |
| In other words: Once you get your vaccine jab, the genetic instructions contained in the mRNA molecules are injected into the upper arm and the ribosomes in the muscle cells translate them to make a critical fragment of the viral protein directly inside your body. This 'preview' of what the real virus looks like gives the immune system time to design powerful antibodies that can neutralize the real virus if it ever gets in contact with it. | |
| The protein production inside the muscle cells initiated by the injected mRNA injection reaches peak levels for 24 to 48 hours and can last for a few more days. Thereafter, the mRNA molecules get disassembled by the body. | |
 |
|
| A comparison of traditional vaccine with the new type of mRNA vaccine. (Image: Vanderbilt Institute for Infection, Immunology and Inflamation) (click on image to enlarge) | |
The revolutionary impact of mRNA technology |
|
| mRNA COVID-19 vaccines have demonstrated in a very convincing way that biotechnologies have entered the industrial age. What we are seeing here is nothing less than the rise of bio platforms that give us the ability to engineer bits of biology, such as mRNA, to create programmable medicines and vaccines. | |
| More generally, if it is indeed possible that mRNA can be used to make the full set of proteins in life, then it becomes possible to treat an incredible broad range of human diseases. This is at the core of the industrialized platforms that Moderna, BioNTech and others are building. | |
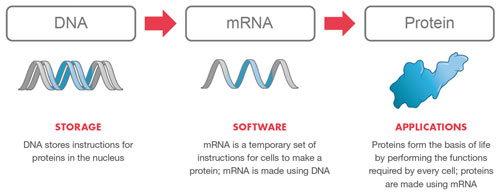
| Essentially, an mRNA technology platform functions very much like an operating system on a computer. It is designed so that it can plug and play interchangeably with different programs. In this case, the 'program' or 'app' is the unique mRNA sequence that codes for a specific protein. | |
| mRNA as the technological basis for therapeutics and vaccines is characterized by a great flexibility with respect to production and application. In essence, mRNA is an information-carrying molecule that can be industrialized – as opposed to traditional therapeutic molecules that have to be elaborately designed and synthesized from scratch for each application (i.e. medicine). | |
| For starters, mRNA molecules are far simpler than proteins. mRNA is manufactured by chemical rather than biological synthesis, so it is much quicker than conventional vaccines to be redesigned, scaled up and mass-produced. | |
| An excellent primer on the development of mRNA-vaccine technologies explains why: "Any protein can be encoded and expressed by mRNA, in principle enabling the development of prophylactic and therapeutic vaccines fighting diseases as diverse as infections and cancer as well as protein replacement therapies." | |
| And this is very the disruptive effect of the mRNA platform happens: If a therapy requires a certain protein to be encoded, only the sequence of the messenger RNA molecule needs to be changed, leaving its physico-chemical characteristics largely unaffected. In the above computer analogy, that is like writing a new piece of software that runs on the same operating system. | |
 |
|
| The mRNA technology platform. (Image: Moderna) | |
The disruptive force of emerging bio platforms |
|
| This means that diverse products can be manufactured using the same established production process – the same equipment, the same operators – without any adjustment and thereby saving massive amounts of time time and money compared with other vaccine or therapeutics platforms. | |
| Having a library of genomes of potentially dangerous viruses, combined with the ability to quickly generate digital copies of emerging viruses thanks to powerful sequencing techniques, makes it possible to rapidly generate digital vaccine designs on a computer. | |
| In the case of BioNTech and Moderna, these two companies spent a decade building their platforms to design and produce mRNA therapeutic candidates at massive scale, although originally targeted towards cancer medicines. | |
| Moderna designed the final version of its vaccine within two days the first SARS-CoV-2 genome sequencing was made public – a matter of swapping out the '4 letters of life' (the four nucleotides), according to CEO Stephane Bancel: "In 48 hours, we designed and locked down the entire chemical structure of the vaccine." | |
| Listen to Moderna CEO Stephane Bancel describing the development of the company's COVID-19 mRNA vaccine. | |
| This same dynamic allowed BioNTech to rapidly redirect its mRNA technology platform from cancer to COVID in a matter of weeks; the company estimates it can manufacture updated versions against emerging mutant strains in as little as six weeks. | |
| What this all boils down to is that in the future every disease or infection can be described as a data sequence and every biological cure as an algorithm. As BioNTech states it: "Considering that all mRNA is generated with four different building blocks, but with unique sequence order, all therapeutic mRNAs have highly similar compositions, while having the capacity to encode a variety of different proteins. These characteristics allow for rapid development of mRNA therapeutics that are broadly applicable for treatment of many diseases, including cancer, infectious diseases and rare diseases." | |
What are the limitations? |
|
| The limitations of mRNA technology are reached when the mechanism of a disease are not well understood, as for instance is the case with HIV, Alzheimer's or many cancers. | |
| However, as soon as you can pinpoint a specific protein, or several proteins in a certain ratio, as the root cause for a disease, then mRNA researchers can get to work on their computers and start designing the instructions for proteins that fix the problem. | |
| Another complicating factor is to design the right delivery vehicle to get the mRNA into the targeted tissue and cells while evading the immune system. For vaccines it is relatively easy to inject it into muscle cells. It gets more difficult to get it to the brain, heart or the lungs. | |
| Also, ribosomes have to think the mRNA was produced naturally, so they can accurately read the instructions to produce the right protein. Finally, the cells need to express enough of the protein to have the desired therapeutic effect. | |
The big picture |
|
| The emerging bio platforms will impact more than just industrialized vaccine development. They will transform all areas of biotechnology: areas like small molecule discovery, protein engineering, genome editing, gene delivery, and cell therapy. | |
| By programming biology to allow a body to make its own medicine – programmable medicine – it will become possible to tailor diagnostics and therapies based on the genetic features of the disease-causing molecules. And because it is all based on the same underlying platform, it will be provided it in an easily reproducible, timely and cost-effective way. | |
| Using mRNA as a platform technology – pretty much what Android or iOS are today for smartphones – will ultimately allow to create 'apps' for target groups such as allergy sufferers or smokers. It might even lead to bio agents that are synthesized for just a single individual, taking the term 'individualized medicine' to its logical conclusion. | |
 By
Michael
Berger
– Michael is author of three books by the Royal Society of Chemistry:
Nano-Society: Pushing the Boundaries of Technology,
Nanotechnology: The Future is Tiny, and
Nanoengineering: The Skills and Tools Making Technology Invisible
Copyright ©
Nanowerk LLC
By
Michael
Berger
– Michael is author of three books by the Royal Society of Chemistry:
Nano-Society: Pushing the Boundaries of Technology,
Nanotechnology: The Future is Tiny, and
Nanoengineering: The Skills and Tools Making Technology Invisible
Copyright ©
Nanowerk LLC
|
|
|
Become a Spotlight guest author! Join our large and growing group of guest contributors. Have you just published a scientific paper or have other exciting developments to share with the nanotechnology community? Here is how to publish on nanowerk.com. |
|
