| Posted: Mar 10, 2015 | |
Has nanomedicine lived up to its promise? |
|
| (Nanowerk Spotlight) In early 2003, the European Science Foundation launched its Scientific Forward Look on Nanomedicine, a foresight study (report here ;pdf) and in 2004, the U.S. National Institute of Health (NIH) published its Roadmap (now Common Fund) of the Nanomedicine Initiative. This program began in 2005 with a national network of eight Nanomedicine Development Centers. Now, in the second half of this 10-year program, the four centers best positioned to effectively apply their findings to translational studies were selected to continue receiving support. | |
| A generally accepted definition of nanomedicine refers to highly specific medical intervention at the molecular scale for curing disease or repairing damaged tissues, such as bone, muscle, or nerve. | |
| Although products classified as nanomedicine products have indeed appeared over the past decade, such products have not exactly revolutionized treatment paradigms as envisaged earlier. | |
| In particular no molecular machine or nanorobot has yet entered clinical trials, although research in these areas is picking up pace. | |
| In a Perspectives article in Nanotechnology ("Has nanomedicine lived up to its promise?"), Professor Subbu Venkatraman, Director of the NTU-Northwestern Nanomedicine Institute in Singapore, takes a look back and tries to recalibrate our expectations. | |
 |
|
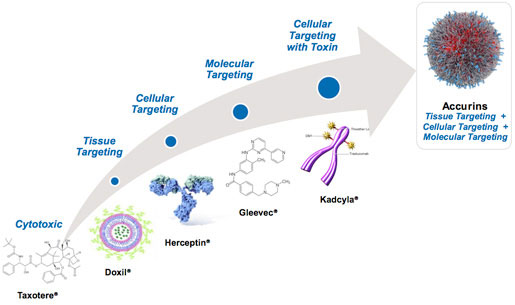
| A multi-functional nanocarrier of promise (as shown on the Bind Therapeutics website). | |
| Here are some numbers: Historically, the approval of Doxil as the very first nanotherapeutic product in 1995 is generally regarded as the dawn of nanomedicine for human use. By 2013, the number of approved products had reached 54 in all, with another 150 in various stages of clinical trials. A PubMed search on articles relating to nanomedicine shows 7400 hits over 10 years, of which 1874 were published in 2013 alone. Similarly, the US patent office database shows 409 patents (since 1976) that were granted in nanomedicine, with another 679 applications awaiting approval. | |
| "So judging by research activity and funding the field of nanomedicine has been very fertile; however, when we use the yardstick of clinical success and paradigm shifts in treatment, the results appear more modest," writes Venkatraman. | |
| Although it is evident that the use of nanotechnology in medicine is widespread, and spans in vitro diagnostics, in vivo imaging and injectable therapeutics, it has not yet led to complete shifts in treatment paradigms – although it is beginning to do so. | |
| "Why has this technology taken so long to bear fruit in medicine?" asks Venkatraman. The answer: Possibly the uncertainty over the environmental consequences of the use of nanotechnology (in handling during manufacture, for example) is one contributing factor; this has necessitated more elaborate safety testing, and consequently led to a longer pre-clinical phase of development, and thus to higher costs of development. | |
| Scaling up of nanomedicine products has also not been straightforward, and has cost time and money. Financing of such projects (with long commercialization times) is subject to a cost-to-benefit analysis, which may have been marginal for many current nanomedicine concepts. | |
| What are the major obstacles to be overcome? | |
| "Given the more stringent safeguards for handling nanoparticles and their perceived toxic effects, I believe that nanotoxicology must take a more central role in product development," writes Venkatraman. "Another important advance is to establish sufficient control over drug efflux from nanocarriers, which is not a trivial task. We must also explore routes of administration other than intra-venous injections." | |
| Additionally, it is important that truly multidisciplinary research drives the solutions to current medical needs, with active participation from clinician scientists at every stage of the process. | |
| Such multidisciplinary nanomedicine centres have been set up worldwide (for example at Northwestern University, University of California at San Diego and Nanyang Technological University, to name a few), and it will be exciting to follow their translational success rates in the future. | |
| In the final analysis, only with demonstrable and superior patient benefits, and overall cost reductions in nanotechnology in healthcare management, can nanomedicine make bigger inroads. | |
 By
Michael
Berger
– Michael is author of three books by the Royal Society of Chemistry:
Nano-Society: Pushing the Boundaries of Technology,
Nanotechnology: The Future is Tiny, and
Nanoengineering: The Skills and Tools Making Technology Invisible
Copyright ©
Nanowerk LLC
By
Michael
Berger
– Michael is author of three books by the Royal Society of Chemistry:
Nano-Society: Pushing the Boundaries of Technology,
Nanotechnology: The Future is Tiny, and
Nanoengineering: The Skills and Tools Making Technology Invisible
Copyright ©
Nanowerk LLC
|
|
|
Become a Spotlight guest author! Join our large and growing group of guest contributors. Have you just published a scientific paper or have other exciting developments to share with the nanotechnology community? Here is how to publish on nanowerk.com. |
|
